Coronavirus: the science in brief Understand article
As scientists worldwide try to understand and help tackle the coronavirus pandemic, we take a brief look at what is currently known about this new virus.
With the recent outbreak of COVID-19, the disease caused by the coronavirus SARS-CoV-2, the news has been ablaze with information, updates and, in some cases, misinformation. This article aims to present a simple account of the science that underpins our developing understanding of this new virus.
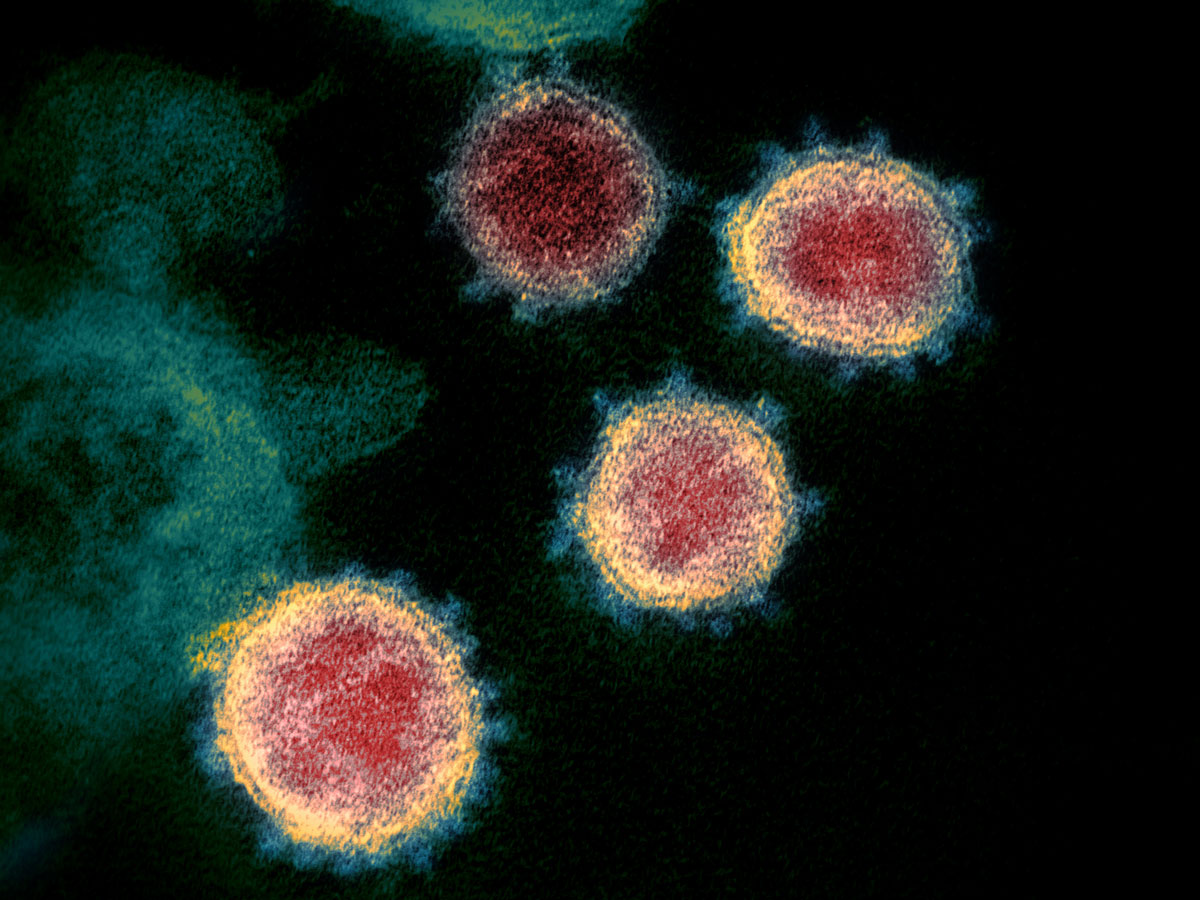
NIAID-RML, CC BY 2.0
What is a coronavirus?
Coronaviruses belong to the family Coronaviridae. ‘Corona’ (which comes from the Greek word for crown) refers to the virus’s characteristic round outer envelope, which is covered with spiky proteins. There are dozens of species in the coronavirus family. They occur worldwide in a range of mammals and birds, but only seven species have infected humans to date. Three of these have caused fatal outbreaks, including the most recent one.
Scientists think close interactions between people and animals triggered all three outbreaks. The rationale behind this theory is that viruses can mutate and adapt to new hosts, allowing them to jump from animals to humans. In some viruses, such as chickenpox, genes are encoded as DNA. Coronaviruses, however, have an RNA genome. RNA viruses generally mutate faster than DNA viruses, because they have a more limited ability to ‘proofread’ their genes as they copy them, leading to a higher rate of errors. As a result, RNA viruses such as influenza and the common cold evolve into new strains every season, making them very difficult to treat or protect against. However, SARS-CoV-2 does show proofreading activity, and so far the virus seems more genetically stable than influenza viruses.
In 2002, a coronavirus called SARS-CoV came to the world’s attention after it mutated and spread to humans from cat-like animals called civets, although its original host was most likely a bat. It caused a dangerous lung disease called severe acute respiratory syndrome (SARS), killing around 10% of people who tested positive for the virus. Ten years later, MERS-CoV (Middle East respiratory syndrome coronavirus) was identified in Saudi Arabia. It too may have originated in bats, but it was spread to humans via camels as the intermediate host (Andersen et al., 2020). Even deadlier than SARS, MERS-CoV had a fatality rate of around 34%.
The latest coronavirus to make the leap from animals to humans, SARS-CoV-2, was first identified in December 2019 in Wuhan, China. It probably also originated in bats and reached humans via an intermediate host. That species has not yet been identified, although some researchers think it may have been the pangolin (scaly anteater).
Reproduction and spread
Like all viruses, SARS-CoV-2 cannot reproduce without invading a living cell. To do so, the virus must first attach to the outer membrane of the cell it is invading. The virus uses the protein molecules that form its spiky crown to attach to specific receptor molecules embedded in the host cell’s surface membrane.
The cell surface receptor molecule used by SARS-CoV and SARS-CoV-2 is the same: a protein called ACE2, which is found in the respiratory tract, especially the lungs. However, researchers have identified a key difference in the SARS-CoV-2 spike protein that may play a role in the high infectivity of the virus. The spike protein needs to be activated by a host protein that cleaves it, and SARS-CoV-2 contains a unique site for cleavage by a host-cell enzyme called furin. This cleavage site is not present in the most closely related bat and pangolin viruses. Furin is found in many tissues and organs in the human body, including the liver, the small intestine and the lungs. This may account for cases in which the virus has spread through the body and damaged multiple organs. It may also increase the infectiousness of SARS-CoV-2.
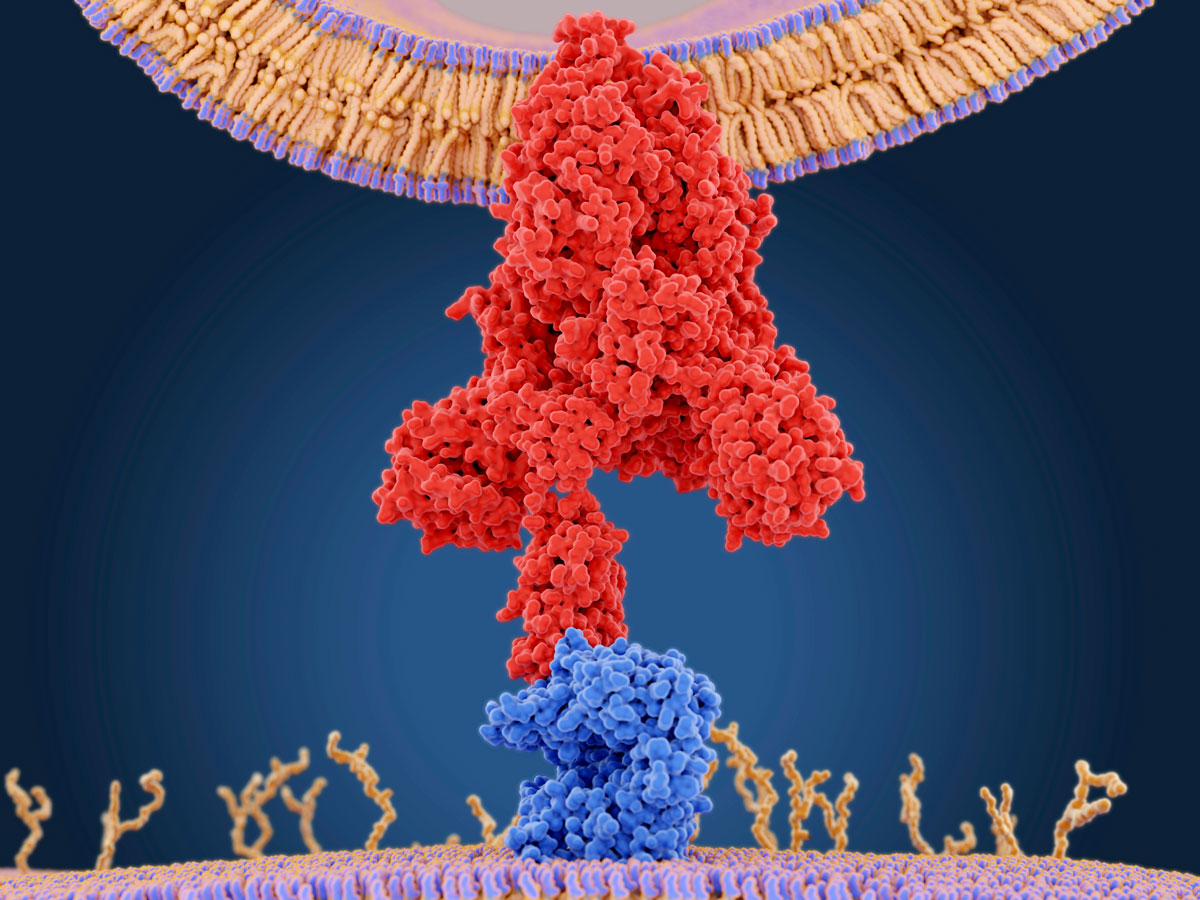
Juan Gartner/Science Photo Library
One of the greatest challenges of SARS-CoV-2 is that many of the people it infects have mild symptoms or no symptoms at all. This not only makes them difficult to identify and isolate but also allows them to remain socially active, spreading the virus. As a result, SARS-CoV-2 is much more infectious than SARS or MERS-CoV-2 (Mallapaty, 2020).
Epidemiologists can model the spread of an infectious disease such as COVID-19 through a population if they know how many people an average person infects. This is known as the reproduction number, or R0. If the R0 is greater than 1, the number of infections grows exponentially, but if the R0 is less than 1, the disease will die out. COVID-19 has an R0 of around 2.2, though estimates vary from 1.4 to 3.9. It’s important to note that the R0 is not an intrinsic property of the virus; it varies with the circumstances. Social distancing, closure of schools, and travel restrictions all lower the R0 of COVID-19. The aim of governments is to reduce the R0 to below 1 and so reverse the trend of ever-rising numbers of infections. Even if the R0 isn’t lowered below 1, any fall in the number reduces the speed of the pandemic’s spread – which, importantly, reduces the strain on health services.
Respiratory infections such as COVID-19 are spread primarily by tiny airborne droplets of mucus released when people cough or sneeze. Anyone within 2 metres or so of an infected person is at significant risk of breathing in these droplets and becoming infected. Droplets may also land on surfaces that people touch, causing them to inadvertently infect the mucous membranes in their mouth, nose or eyes when touching the face – something we do up to 20 times an hour (Kwok et al., 2015). Research has shown that the virus SARS-CoV-2 can stay airborne for several hours and remains viable for up to 24 hours on cardboard, two days on plastic, and three days on stainless steel (van Doremalen et al., 2020).
Fighting the COVID-19 pandemic
There are many ways that people can help to lower the R0 of COVID-19 and so help to combat the pandemic. For example, one important precaution to reduce transmission is to cover the mouth and nose with a bent elbow or tissue when sneezing or coughing.
Frequent handwashing also helps, especially if it is done thoroughly. Some false reports have declared that sanitisers and soaps have little to no effect on the virus, but this couldn’t be further from the truth. Coronaviruses are destroyed by handwashing, because detergents such as soap attack the lipid membrane that forms the virus’s outer envelope. Alcohol-based sanitisers have the same effect, but there are key differences in the way soap and sanitisers should be used. Soapy water is very effective at removing particles of dirt and grease that can harbour and protect viruses. This is why scrubbing your hands thoroughly is important. (Normally, around 30% of people don’t routinely wash their hands after visiting the bathroom, and of those who do, only 50% wash their hands correctly.)
Sanitisers don’t clean the skin, but they do inactivate the virus if the alcohol makes contact with its outer envelope. Although they are less effective than soap and water, hand sanitisers are quicker and more convenient. They are also a good option for people who do not have access to proper handwashing facilities or who have to continually maintain hand hygiene, such as people in the health services (Hall, 2012).
A flu pandemic model developed in 2018 by epidemiologists at University College London suggested that handwashing alone could reduce transmission by 22% (Corcoran, 2020). It is not a direct model for COVID-19, but it does demonstrate how everyone has a part to play in protecting the wider population, as well as ourselves, when we are faced with a pandemic.

Maridav/Shutterstock
Acknowledgement
The authors would like to thank Science Foundation Ireland (SFI) for funding their work on writing this article, under grant agreement number 12/RC/2275_P2.
References
- Andersen KG et al. (2020) The proximal origin of SARS-CoV-2. Nature Medicine 26: 450-452. doi: 10.1038/s41591-020-0820-9
- Corcoran K (2020) A pandemic simulation from 2018 shows how washing your hands more often could slow down an outbreak like the coronavirus. Business Insider 7 March 2020
- Hall J (2012) Do hand sanitizers really work? University of Toronto News 10 January 2012
- Kwok YLA, Gralton J, McLaws ML (2015) Face touching: A frequent habit that has implications for hand hygiene. American Journal of Infection Control 43(2): 112-114. doi: 10.1016/j.ajic.2014.10.015
- Mallapaty S (2020) Why does the coronavirus spread so easily between people? Nature 579: 183. doi: 10.1038/d41586-020-00660-x
- van Doremalen N et al. (2020) Aerosol and surface stability of HCoV-19 (SARS-CoV-2) compared to SARS-CoV-1. New England Journal of Medicine doi: 10.1056/NEJMc2004973
Resources
- Explore some of the key coronavirus questions in this article from Science News.
- Find out more about viruses – ‘bad news wrapped in protein’ – and how they are able to force infected cells to replicate the virus.
- Read this article from Science News for Students that clearly explains some key concepts, written when the SARS-CoV-2 pandemic was at a relatively early stage.
- Find out more about the reproduction number R0 in this article from the University of Michigan, USA.
- Learn about how genetic sequencing helps to track the route of virus transmission in this accessible article from Science.
- Get the latest information about the SARS-CoV-2 pandemic from the World Health Organization’s interactive map.
- Read about the science behind why handwashing is so important in this article from Smithsonian magazine.
- Learn more about the science of hand sanitisers.
- Find out how soap kills coronaviruses in this article from The Guardian newspaper.





