Guardian of the brain: the blood-brain barrier Understand article
Insights into the brain’s unique protective barrier could offer promising treatments for diseases such as multiple sclerosis and Alzheimer’s.
When the German scientist Paul Ehrlich injected dye into the bloodstream of mice more than 130 years ago, he came across an unusual phenomenon. The dye slowly spread across the tissue, staining every organ except one – the brain. Although Ehrlich’s staining experiments would eventually culminate in his discovery of the first chemotherapy drug to treat syphilis – and earn him a Nobel Prize – this particular result puzzled him. He suggested that this lack of staining was due to the brain tissue taking up less dye.
Tatiana Shepeleva/Shutterstock.com
When one of his students, Edwin Goldman, injected the dye directly into the brain instead, the explanation became more obvious. The opposite effect occurred: only the brain was stained, and the other organs were spared (see figure 1). This was the first indication of the blood-brain barrier – first termed Blut-Hirn-Schranke in German – separating the circulating blood from the brain and spinal cord of the central nervous system (CNS). It was not until the introduction of electron microscopy in the 1960s that this barrier was precisely located, and the tightly woven ultrastructure of the cells responsible became visible.
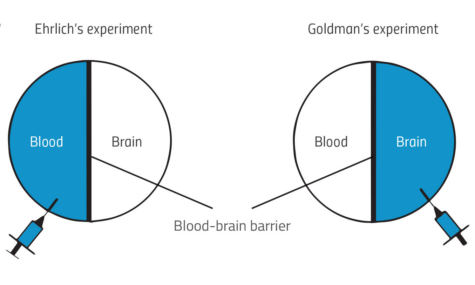
Yun Jiang
What is the blood-brain barrier?
Our understanding of the brain – arguably the most important and sensitive organ in the human body – is still far from complete. But our knowledge of the blood-brain barrier has advanced considerably since Ehrlich’s time.
Throughout the body, endothelial cells line the inner surface of blood vessels and lymphatic vessels. Endothelial cells, for example, control the exchange of substances between circulating blood and the surrounding tissue. The brain, however, needs special care and protection, because many substances that are harmless to other organs could be toxic to the CNS. For instance, some proteins in the plasma – such as albumin and immunoglobulin – can cause inflammation in the nervous system.
To stop these substances reaching the brain, specialised endothelial cells form a barrier to restrict the movement of substances from the circulating blood to the extracellular fluid in the CNS. The key difference between these cells and normal endothelial cells is how they are stitched together.
Tight junctions
A variety of special seals, known as tight junctions, connect the spaces between adjacent brain endothelial cells. The tight junctions are formed by proteins that span the cell membranes. Inside the cells, the proteins are anchored to the cytoskeleton (a network of fibres within a cell that helps gives the cell its shape), whereas outside the cell, they interact with the other tight junction proteins of neighbouring cells. Like double-sided tape, the tight junctions stick two cells together to prevent the passage of most molecules and ions through the space between the cells (see figure 2).
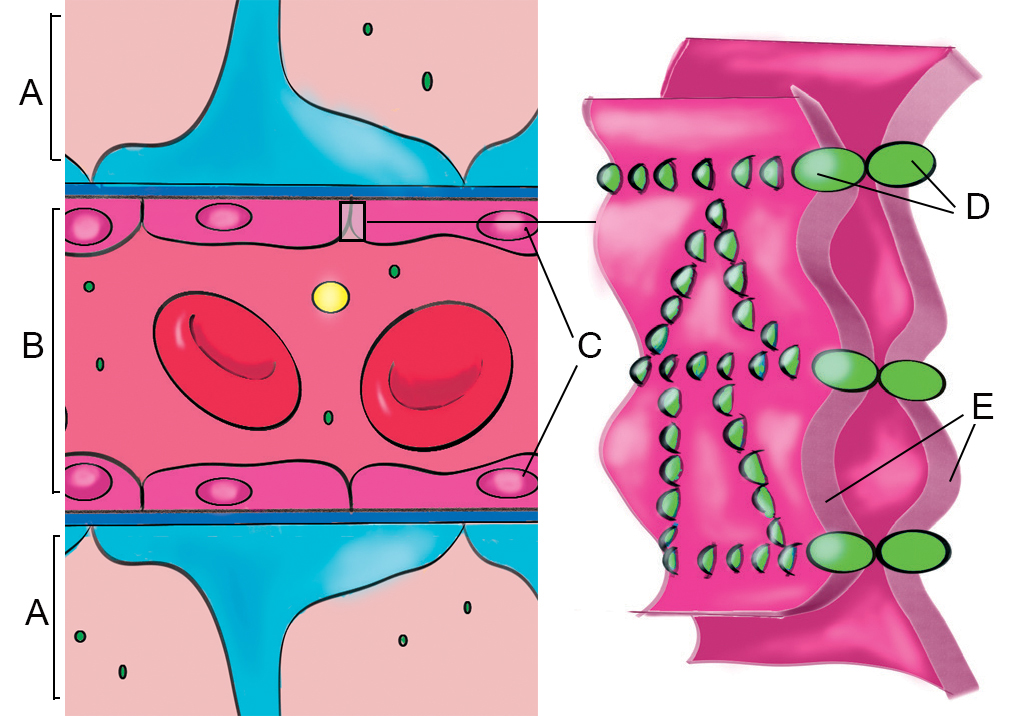
Yun Jiang
Only some small molecules (water; certain gases such as oxygen and carbon dioxide) and lipid-soluble substances (such as small fatty acids) can move passively through the barrier. Other selected molecules, such as glucose, must be transported by specialised transport proteins embedded in the cell membranes. Thus, the brain’s microenvironment is maintained so that the nervous system functions optimally and the CNS is protected from harmful substances.
Besides the tight endothelium, neurons and other specialised non-neuronal cells (such as astrocytes and microglia) orchestrate the function of the blood-brain barrier (see figure 3). Together with endothelial cells, they form a dynamic structure called the neurovascular unit (NVU). If any of the cells in the NVU fail, the barrier breaks down.
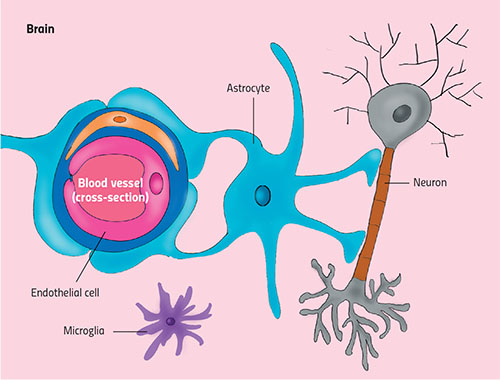
Yun Jiang
The blood-brain barrier and neurological diseases
Various disorders, such as infection or trauma, can damage the tight junctions and the NVU, disrupting the tightly knitted structure of the blood-brain barrier. When this happens, the formerly controlled flux of molecules and ions in and out of the brain becomes erratic. Toxins, pathogens or cells of the immune system might enter the brain, causing the CNS to become inflamed. In response, cells release related cytokines – substances that are secreted following inflammation or immune system activity. This disrupts the neurons and causes them to degenerate, leading to the development of neurological diseases.
One such disease is multiple sclerosis (MS), an autoimmune disorder in which the immune system attacks the CNS. Patients experience numb arms and legs, sensations of electric shocks and problems with their vision. The development of MS is complicated, but changes to the blood-brain barrier are believed to play an important role. Scientists think that some initial inflammatory responses help to increase the permeability of the barrier, which allows immune cells to invade the brain. This boosts the inflammatory responses in the CNS, which further disrupts the barrier and increases the damage to nerve cells.
Therapies for the future
Many studies have shown the link between the disruption of the blood-brain barrier and other neurological diseases, including stroke, epilepsy, Alzheimer’s disease and Parkinson’s disease. Scientists therefore believe that enhancing the repair of a damaged blood-brain barrier is a good strategy for treating neurological diseases.
One example of such treatment is the use of a steroid hormone called glucocorticoid, which reduces the unwanted inflammatory responses and is believed to influence the formation of tight junctions. Glucocorticoid has been shown to repair the blood-brain barrier in both MS patients and related mouse models (Salvador et al., 2014). However, this hormone may not be suitable for using as a long-term treatment due to its side effects, which include mood changes, gastrointestinal problems and high blood-sugar levels (Ciriaco et al., 2013; Liu et al., 2013).
Nevertheless, other potential therapies are still under investigation. Transplanting a type of progenitor cell that can generate new endothelial cells, for example, could help to reconstruct the blood-brain barrier following stroke (Kaneko et al., 2012). As studies continue, a deeper understanding of the disruption and repair of the blood-brain barrier will offer more options for the treatment of related neurological diseases
References
- Ciriaco M et al. (2013) Corticosteroid-related central nervous system side effects. Journal of Pharmacology and Pharmacotherapeutics 4(S1): S94-S98. doi: 10.4103/0976-500X.120975
- Kaneko Y et al. (2012) Cell therapy for stroke: emphasis on optimizing safety and efficacy profile of endothelial progenitor cells. Current Pharmaceutical Design 18(25): 3731-3734. doi: 10.2174/138161212802002733
- Liu D et al. (2013) A practical guide to the monitoring and management of the complications of systemic corticosteroid therapy. Allergy, Asthma & Clinical Immunology 9(1): 30. doi: 10.1186/1710-1492-9-30
- Salvador E, Shityakov S, Förster C (2014) Glucocorticoids and endothelial cell barrier function. Cell and Tissue Research 355(3): 597-605. doi: 10.1007/s00441-013-1762-z
Resources
- For an introduction to the blood-brain barrier for children, visit the University of Washington website.
- For a further introduction about the blood-brain barrier and the neurovascular unit, watch these videos on YouTube: ‘Blood Brain Barrier‘, and ‘2-Minute Neuroscience: Blood-Brain Barrier‘.
Review
This article elegantly describes an observation made over 100 years ago of the distribution of a dye and the conclusion that there is a physical barrier that protects the brain. The article is engaging as it inspires the reader to reflect on the anatomically and functionally unique structure of the blood-brain barrier.
The link between damage to the blood-brain barrier and neurological diseases is important as this could lead to advances in the treatment of central nervous system diseases. The focus on multiple sclerosis is relevant given that it is the most common neurological disability among young people.
The article is useful for background reading and comprehension exercises. It could also be used for discussions such as the use of stem cells to repair the blood-brain barrier. There is potential for the article to form a starting point for extended essays.
Questions about the article could include:
- What specialisations allow the endothelial cells to form tight junctions?
- How are molecules transported across the blood-brain barrier?
- List the factors that might disrupt normal functioning of the blood-brain barrier.
- Is the term blood-brain barrier appropriate, as evidence shows it is a dynamic structure allowing controlled passage of molecules?
Dr Mary Brenan, biology teacher, Concord College, UK





